The study of relationships between bladder volume and intravesical prostatic protrusion on transabdominal ultrasound in patients with benign prostatic hyperplasia
DOI:
https://doi.org/10.46475/asean-jr.v27i1.994Keywords:
Benign prostatic hyperplasia, Bladder volume, Intravesical prostatic protrusion, Prostate volume, Post-void residualAbstract
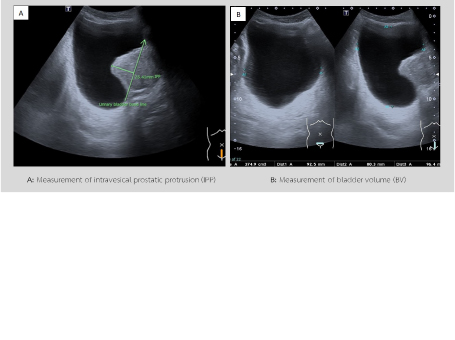
Background: Benign prostatic hyperplasia (BPH) is a common cause of lower urinary tract symptoms (LUTS) in ageing men, primarily resulting from bladder outlet obstruction (BOO). Intravesical prostatic protrusion (IPP), assessed by transabdominal ultrasonography, has emerged as a reliable and non-invasive imaging marker reflecting the degree of BOO. However, IPP measurements may vary with bladder volume (BV), and the optimal filling level for consistent evaluation remains uncertain.
Objective: To examine the relationships between IPP, BV, prostate volume (PV), postvoid residual urine (PVR), and symptom severity (IPSS) in patients with BPH.
Materials and methods: A prospective cohort study was conducted at xxxx, from May to October 2025. Fifty-four men aged ≥50 years with ultrasonographically confirmed BPH underwent four standardised transabdominal ultrasound scans: three for BV, PV, and IPP, and one for PVR. Baseline IPSS was recorded. Pearson correlation and group comparisons were performed, with statistical significance defined as p < 0.05.
Results: IPP demonstrated significant positive correlations with PV (p = 0.007) and PVR (p < 0.001), but not with BV (p = 0.762) or IPSS (p = 0.887). Patients with Grade 3 IPP had the largest PV and highest PVR (p = 0.038 and p = 0.016).
Conclusion: IPP was significantly associated with PV and PVR but not with IPSS. Measurements were most consistent at bladder volumes of 200–299 mL, underscoring the importance of standardised bladder filling for accurate IPP assessment.
Keywords: Benign prostatic hyperplasia, Bladder volume, Intravesical prostatic protrusion, Prostate volume, post-void residual.
Downloads
References
GBD 2019 Benign Prostatic Hyperplasia Collaborators. The global, regional, and national burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Healthy Longev 2022;3:e754–76. doi: 10.1016/S2666-7568(22)00213-6.
Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep 2017;7:7984. doi:10.1038/s41598-017-06628-8.
Institute for Population and Social Research, Mahidol University. Thai Health 2023 : Thailand’s Commitment in COP (Conference of Parties) & Responses to Climate Change [Internet]. Nakhon Pathom: Institute for Population and Social Research, Mahidol University with Thai Health Promotion Foundation; 2023 [cited 2025 Feb 11]. Available from: https://bps.moph.go.th/new_bps/sites/default/files/statistic53.pdf
Chunhakrai V, Santingamkun A, editors. Common urologic problems for medical student [Internet]. Bangkok: Thai Urological Association under The Royal Patronage; 2015. Thai. [cited 2025 Dec 26]. Available from: https://www.tuanet.org/wp-content/uploads/2020/06/07_Common-Urologic-Problems.pdf
Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline part I—initial work-up and medical management. J Urol 2021;206:806–17. doi:10.1097/JU.0000000000002183.
European Association of Urology. EAU Guidelines on Management of Male LUTS [Internet]. Arnhem (The Netherlands): EAU; 2013 [cited 2025 Feb 11]. Available from: https://uroweb.org/guidelines
Rosier PFWM, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, et al. International Continence Society good urodynamic practices and terms 2016: urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn 2017;36:1243–60. doi:10.1002/nau.23124.
Eze BU. Intravesical prostatic protrusion as a predictor of need for surgical therapy in benign prostatic hyperplasia patients. EJMED [Internet]. 2023 [cited 2025 Dec 27];5:9–12. Available from: https://eu-opensci.org/index.php/ejmed/article/view/41746
Al Rashed AA, Isa QM, Mahdi A, Ebrahim M, Abdulaziz K, Hasan O, et al. Clinical outcomes of intravesical prostatic protrusion in patients with benign prostatic hyperplasia. Cureus 2024;16:e52541. doi:10.7759/cureus.52541.
Lee LS, Sim HG, Lim KB, Wang D, Foo KT. Intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. Int J Urol 2010;17:69–74. doi:10.1111/j.1442-2042.2009.02409.x.
Hossain AK, Alam AK, Habib AK, Rashid MM, Rahman H, Islam AK, et al. Comparison between prostate volume and intravesical prostatic protrusion in detecting bladder outlet obstruction due to benign prostatic hyperplasia. Bangladesh Med Res Counc Bull 2012;38:14–7. doi:10.3329/bmrcb.v38i1.10446.
Yuen JS, Ngiap JT, Cheng CW, Foo KT. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol 2002;9:225–9. doi:10.1046/j.1442-2042.2002.00453.x.
Gandhi J, Weissbart SJ, Kim AN, Joshi G, Kaplan SA, Khan SA. Clinical considerations for intravesical prostatic protrusion in the evaluation and management of bladder outlet obstruction secondary to benign prostatic hyperplasia. Curr Urol 2018;12:6–12. doi:10.1159/000447224.
Esomonu U, Obun C, Ude R, Igwe S, Esomchi C, Ogolekwu S. Prevalence of benign prostatic hyperplasia and prostate cancer among suburban residents in southern Nigeria. Afr J Urol 2024;30:66. doi:10.1186/s12301-024-00470-x.
Wayne DW. Biostatistics: a foundation for analysis in the health sciences. 7th ed. New York: John Wiley & Sons; 1995.
Iwenofu CA, Amu OC, Affusim EA, Nwachukwu CD, Anyimba SK. Correlation of intravesical prostatic protrusion with severity of lower urinary tract symptoms in men with symptomatic benign prostatic hyperplasia at University of Nigeria Teaching Hospital, Ituku-Ozalla Enugu. Niger J Med 2024;33:19–24. doi:10.4103/NJM.NJM_110_23.
Ruamcharoen S. Benign prostatic hyperplasia at Nakhon Phanom Hospital. Sanpasitthiprasong Med J 2021;35(1):1–12. Thai.
Wang D, Huang H, Law YM, Foo KT. Relationships between prostatic volume and intravesical prostatic protrusion on transabdominal ultrasound and benign prostatic obstruction in patients with lower urinary tract symptoms. Ann Acad Med Singap 2015;44:60–5.
Shin SH, Kim JW, Kim JW, Oh MM, Moon du G. Defining the degree of intravesical prostatic protrusion in association with bladder outlet obstruction. Korean J Urol 2013;54:369–72. doi:10.4111/kju.2013.54.6.369.
Lee A, Lee HJ, Lim KB, Huang HH, Ho H, Foo KT. Can intravesical prostatic protrusion predict bladder outlet obstruction even in men with good flow? Asian J Urol 2016;3:39–43. doi:10.1016/j.ajur.2015.10.002.
Kurnia IC, Ghinorawa T, Rochadi S. Correlation of PSA, PV, and IPP in detecting bladder outlet obstruction caused by prostate enlargement. Indones J Urol 2014;21:1–6.
Tan YG, Teo JS, Kuo TLC, Guo L, Shi L, Shutchaidat V, et al. A systematic review and meta-analysis of transabdominal intravesical prostatic protrusion assessment in determining bladder outlet obstruction and unsuccessful trial without catheter. Eur Urol Focus 2022;8:1003–14. doi:10.1016/j.euf.2021.09.016.
Chia SJ, Heng CT, Chan SP, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int 2003;91:371–4. doi:10.1046/j.1464-410x.2003.04088.x.
Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology 2007;70:1096–9. doi:10.1016/j.urology.2007.08.008.
Foo KT. Pathophysiology of clinical benign prostatic hyperplasia. Asian J Urol 2017;4:152–7. doi:10.1016/j.ajur.2017.06.003.
Sigdel G, Belokar W. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic hyperplasia. J Univ Coll Med Sci 2015;3:6–10. doi:10.3126/jucms.v3i1.13248.
Brakohiapa EK, Botwe BO, Sarkodie BD. Prostate volume determination by transabdominal ultrasonography: does accuracy vary significantly with urinary bladder volumes between 50 to 400 mL? J Med Radiat Sci 2019 ;66:81-90. doi: 10.1002/jmrs.320.
Chauhan K, Ebner DK, Tzou K, Ryan K, May J, Kaleem T, et al. Assessment of bladder filling during prostate cancer radiation therapy with ultrasound and cone-beam CT. Front Oncol 2023;13:1200270. doi:10.3389/fonc.2023.1200270.
Hynds S, McGarry CK, Mitchell DM, Early S, Shum L, Stewart DP, et al. Assessing the daily consistency of bladder filling using an ultrasonic bladderscan device in men receiving radical conformal radiotherapy for prostate cancer. Br J Radiol 2011;84:813–8. doi:10.1259/bjr/50048151.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 The ASEAN Journal of Radiology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Disclosure Forms and Copyright Agreements
All authors listed on the manuscript must complete both the electronic copyright agreement. (in the case of acceptance)