Factors related to bone mineral density in female patients receiving TSH-suppressive doses of levothyroxine for thyroid cancer
DOI:
https://doi.org/10.46475/asean-jr.v24i2.191Keywords:
Bone mineral density, BMD, thyroid cancer, high dose of thyroid hormone, SH-suppressive dose of LT4Abstract
Background: Patients with thyroid cancer receive a high-dose thyroid hormone therapy after total thyroidectomy for suppression of thyroid stimulating hormone (TSH); this may affect bone mineral density (BMD). Identifying the common factors that affect BMD (including the duration of a high dose of thyroid hormone treatment) may, therefore, aid the delivery of appropriate and comprehensive care in such cases.
Objective: To identify the factors related to BMD in female patients with thyroid cancer.
Materials and Methods: This cross-sectional study evaluated data pertaining to the BMD and demographic characteristics of female patients with thyroid cancer. The patients were aged at least 40 years and received a high-dose thyroid hormone replacement therapy after total thyroidectomy at the Rajavithi Hospital between January 2004 and December 2019. The relationships between BMD and associated factors were analyzed using Pearson’s correlation and multiple linear regression. A p-value of less than 0.05 was considered statistically significant.
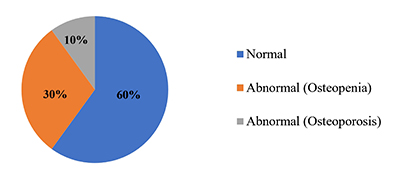
Results: A total of 100 female patients with a mean age of 55.37 ± 11.36 (40-82) years and mean body mass index (BMI) of 24.8 ± 4.96 (15-40) were included; 60 and 56 of them were postmenopausal and coffee drinkers, respectively. High-dose thyroid hormone replacement therapy was received for a mean duration of 94.59±50.36 (3-210) months and 13 patients had a history of fractures; 60%, 30%, and 10% had normal BMD, osteopenia, and osteoporosis, respectively. The factors affecting BMD included the BMI (p-value <0.001) and postmenopausal status(p-value <0.001). Subgroup analyses showed the BMI to be the factor affecting BMD in the premenopausal group (p-value <0.001). Age, BMI, and calcium supplement intake were found to have an effect on the BMD in the postmenopausal group (p-value= 0.003, 0.002, and 0.020, respectively). The duration of high-dose thyroid hormone intake had no effect on the BMD in both the overall population (p-value= 0.558) and the subgroups based on the menopausal status (p-value = 0.437 and 0.380 in premenopausal and postmenopausal groups, respectively).
Conclusion: In female patients who were treated for thyroid cancer, the factors affecting the BMD included the BMI in the premenopausal group and the age, BMI, and calcium supplementation in the postmenopausal group.
Downloads
Metrics
References
Zhang P, Xi H, Yan R. Effects of thyrotropin suppression on lumbar bone mineral density in postmenopausal women with differentiated thyroid carcinoma. Onco Targets Ther 2018;11: 6687-92. doi: 10.2147/OTT.S171282. DOI: https://doi.org/10.2147/OTT.S171282
Thangwijitra S, Sakondhavat C, Soontrapa S, Kaewrudee S, Somboonporn W. Prevalence of osteoporosis in postmenopausal women at Srinagarind Hospital, Khon Kaen University. Thai J Obstet Gynaecol 2010;18:26-34. DOI: https://doi.org/10.1016/S0378-5122(09)70374-3
Johnell O. The socioeconomic burden of fractures: today and in the 21st century. Am J Med 1997;103:20S-5S. doi: 10.1016/s0002-9343(97)90023-1. DOI: https://doi.org/10.1016/S0002-9343(97)90023-1
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 2001;12:417-27. doi: 10.1007/s001980170112. DOI: https://doi.org/10.1007/s001980170112
Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 2004;15:897-902. doi: 10.1007/s00198-004-1627-0. DOI: https://doi.org/10.1007/s00198-004-1627-0
Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA. The human cost of fracture. Osteoporos Int 2005;16:2046-52. doi: 10.1007/s00198-005-1997-y. DOI: https://doi.org/10.1007/s00198-005-1997-y
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-33. doi: 10.1007/s00198-006-0172-4. DOI: https://doi.org/10.1007/s00198-006-0172-4
Suriyawongpaisal P, Siriwongpairat P, Loahachareonsombat W, Angsachon T, Kumpoo U, Sujaritputtangkul S, et al. A multicenter study on hip fractures in Thailand. J Med Assoc Thai 1994;77:488-95.
Suriyawongpaisal P, Chariyalertsak S, Wanvarie S. Quality of life and functional status of patients with hip fractures in Thailand. Southeast Asian J Trop Med Public Health 2003;34:427-32.
Chariyalertsak S, Suriyawongpisal P, Thakkinstain A. Mortality after hip fractures in Thailand. Int Orthop 2001;25:294-7. doi: 10.1007/s002640100270. DOI: https://doi.org/10.1007/s002640100270
Woratanarat P, Wajanavisit W, Lertbusayanukul C, Loahacharoensombat W, Ongphiphatanakul B. Cost analysis of osteoporotic hip fractures. J Med Assoc Thai 2005;88 Suppl 5:S96-104.
Pongchaiyakul C, Songpattanasilp T, Taechakraichana N. Burden of osteoporosis in Thailand. J Med Assoc Thai 2008;91:261-7. DOI: https://doi.org/10.1111/j.1756-185X.2008.00393.x
Bassett JH, Williams GR. Role of Thyroid Hormones in Skeletal Development and Bone Maintenance. Endocr Rev 2016;37:135–87. doi: 10.1210/er.2015-1106. DOI: https://doi.org/10.1210/er.2015-1106
Hillier TA, Cauley JA, Rizzo JH, Pedula KL, Ensrud EK, Bauer DC, et al. WHO Absolute Fracture Risk Models (FRAX): Do Clinical Risk Factors Improve Fracture Prediction in Older Women Without Osteoporosis? J Bone Miner Res 2011;26:1774-82. doi: 10.1002/jbmr.372. DOI: https://doi.org/10.1002/jbmr.372
Kanis JA, Johansson H, Harvey NC, McCloskey EV. A brief history of FRAX. Arch Osteoporos 2018;13:118. doi: 10.1007/s11657-018-0510-0. DOI: https://doi.org/10.1007/s11657-018-0510-0
Daniel WW.. Biostatistics: A foundation of analysis in the health sciences. 6th ed. New York: John Wiley and Sons; 1995. DOI: https://doi.org/10.2307/2533362
Kim CW, Hong S, Oh SH, Lee JJ, Han JY, Hong S, et al. Change of bone mineral density and biochemical markers of bone turnover in patients on suppressive levothyroxine therapy for differentiated thyroid carcinoma. J Bone Metab 2015; 22:135-41. doi: 10.11005/jbm.2015.22.3.135. DOI: https://doi.org/10.11005/jbm.2015.22.3.135
Limpaphayom KK, Taechakraichana N, Jaisamrarn U, Bunyavejchevin S, Chaikittisilpa S, Poshyachinda M, et al. Bone mineral density of lumbar spine and proximal femur in normal Thai women. J Med Assoc Thai 2000;83:725-31.
de Melo TG, da Assumpção LV, Santos Ade O, Zantut-Wittmann DE.. Low BMI and low TSH value as risk factors related to lower bone mineral density in postmenospausal women under levothyroxine therapy for differentiated thyroid carcinoma. Thyroid Res 2015;8:7. doi: 10.1186/s13044-015-0019-1. DOI: https://doi.org/10.1186/s13044-015-0019-1
Fawzy T, Muttappallymyalil J, Sreedharan J, Ahmed A, Alshamsi SO, Al Ali MS, et al. Association between body mass index and bone mineral density in patients referred for dual-energy x-ray absorptiometry scan in Ajman, UAE. J Osteoporos 2011; 2011:876309. doi: 10.4061/2011/876309. DOI: https://doi.org/10.4061/2011/876309
Hariri AF, Almatrafi MN, Zamka AB, Babaker AS, Fallatah TM, Althouwaibi OH, et al. Relationship between body mass index and t-scores of bone mineral density in the hip and spine regions among older adults with diabetes: a retrospective review. J Obes 2019;2019:9827403. doi: 10.1155/2019/9827403. DOI: https://doi.org/10.1155/2019/9827403
Ma M, Feng Z, Liu X, Jia G, Geng B, Xia Y. The saturation effect of body mass index on bone mineral density for people over 50 years old: a cross-sectional study of the US population. Front Nutr 2021;8:763677. doi: 10.3389/funt.2021.763677. DOI: https://doi.org/10.3389/fnut.2021.763677
Finkelstein JS, Brockwell SE, Mehta V, Greendale GA, Sowers MR, Ettinger B, et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab 2008;93:861-8. doi:10.1210/jc.2007-1876. DOI: https://doi.org/10.1210/jc.2007-1876
Chen CH, Chen JF, Yang BY, Liu RT, Tung SC, Chien WY, et al. Bone mineral density in women receiving thyroxine suppressive therapy for differentiated thyroid carcinoma. J Formos Med Assoc 2004;103:442-7.
Kung AW, Yeung SS. Prevention of bone loss induced by thyroxine suppressive therapy in postmenopausal women: the effect of calcium and calcitonin. J Clin Endocrinol Metab 1996; 81:1232-6. doi: 10.1210/jcem.81.3.8772604. DOI: https://doi.org/10.1210/jc.81.3.1232
Chang MC. Bone mineral density in thyroid cancer patients: data from the Korea National Health and Nutrition Examination Survey. J Endocr Surg 2017;17(4):153-9. DOI: https://doi.org/10.16956/jes.2017.17.4.153
Ongphiphadhanakul B, Puavilai G, Rajatanavin R. Effect of TSH-suppressive doses of levothyroxine on bone mineral density in Thai women. J Med Assoc Thai 1996; 79:563-7.
Mazokopakis EE , Starakis IK, Papadomanolaki MG, Batistakis AG, Papadakis JA. Changes of bone mineral density in pre-menopausal women with differentiated thyroid cancer receiving L-thyroxine suppressive therapy. Curr Med Res Opin 2006; 22:1369-73. doi: 10.1185/030079906X115612. DOI: https://doi.org/10.1185/030079906X115612
Yoon BH, Lee Y, Oh HJ, Kim SH, Lee YK. Influence of thyroid-stimulating hormone suppression therapy on bone mineral density in patients with differentiated thyroid cancer: a meta-analysis. J Bone Metab 2019;26:51-60. doi: 10.11005/jbm.2019.26.1.51. DOI: https://doi.org/10.11005/jbm.2019.26.1.51
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The ASEAN Journal of Radiology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Disclosure Forms and Copyright Agreements
All authors listed on the manuscript must complete both the electronic copyright agreement. (in the case of acceptance)