Effect of hepatocellular carcinoma conspicuity on ultrasound on the treatment outcome of percutaneous tumor ablation
DOI:
https://doi.org/10.46475/asean-jr.v26i2.934Keywords:
Fusion ultrasound, Hepatocellular carcinoma, Microwave ablation, Radiofrequency ablation, Tumor ablationAbstract
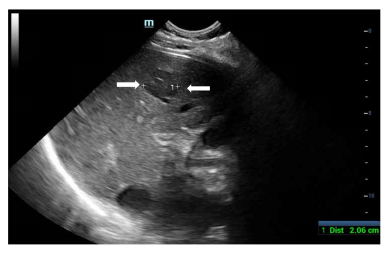
Background: Percutaneous tumor ablation is a minimally invasive treatment for early-stage hepatocellular carcinoma (HCC) and relies on real-time ultrasonographic guidance. However, it might not be feasible in some patients due to limitations of grey-scale ultrasound findings.
Objective: To evaluate the effect of ultrasound conspicuity of HCC nodules on the success rate of percutaneous image-guided ablation
Materials and methods: A single-center retrospective review of patients undergoing percutaneous tumor ablation of treatment-naïve HCC from January 2017 to December 2022 was performed. Three groups of tumors were classified based on the level of ultrasound visualization as complete visibility (399 lesions), partial visibility (219 lesions) and invisibility (88 lesions). Ablation procedure was performed under ultrasound guidance, supplemented with other modalities such as non-contrast CT and fusion ultrasound. Follow-up assessments were conducted at 1, 3, and 24 months post-ablation to compare the technical success rates. Other outcomes including survival analysis and complications were also investigated.
Results: A total of 447 patients with 706 lesions were included. The mean size of lesions in the three groups were 1.84, 1.59, and 1.11 cm, respectively, with statistically significant difference between the groups (p<0.001). There was no statistically significant difference in technical success rates at 1 month or primary efficacy at 3 months among the three groups. The technical success rate between the complete visibility, partial visibility, and invisible groups were 95.7%, 95.0%, and 97.7% (p=0.862), respectively and primary efficacy rates were 95.2%, 95.0%, 84.1% (p=0.172), respectively. The cumulative local tumor progression-free survival at 6, 12, 24 months were 98.0%, 96.9%, and 90.5% for the complete visibility group, 98.9%, 97.9%, and 87.8% for the partial visibility group, and 96.2%, 94.5%, and 87.3% for the invisible group, respectively, with no statistically significant differences (p = 0.539). Only one patient experienced a complication that required further treatment.
Conclusion: The usage of other imaging modalities such as non-contrast CT and fusion ultrasound for poorly conspicuous HCC lesions can improve the success rates to levels comparable with those of the conspicuous nodules, while also maintaining similar local tumor control outcomes and avoiding major adverse events.
Downloads
Metrics
References
Chonprasertsuk S, Vilaichone RK. Epidemiology and treatment of hepatocellular carcinoma in Thailand. Jpn J Clin Oncol 2017;47:294-7. doi: 10.1093/jjco/hyw197. DOI: https://doi.org/10.1093/jjco/hyw197
Reig M, Forner A, Rimola J, Fuster J, Ayuso C, Bruix J, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol 2022; 76: 681-93. doi: 10.1016/j.jhep.2021.11.018. DOI: https://doi.org/10.1016/j.jhep.2021.11.018
Lee MW, Kim YJ, Park HS, Yu NC, Jung SII, Ko SY, et al. Targeted sonography for small hepatocellular carcinoma discovered by CT or MRI: factors affecting sonographic detection. AJR Am J Roentgenol 2010;194:396-400. doi: 10.2214/AJR.09.3171. DOI: https://doi.org/10.2214/AJR.09.3171
Rhim H, Lee MH, Kim YS, Choi D, Lee WJ, Lim HK. Planning sonography to assess the feasibility of percutaneous radiofrequency ablation of hepatocellular carcinomas. AJR Am J Roentgenol 2008;190:1324-30. doi: 10.2214/AJR.07.2970. DOI: https://doi.org/10.2214/AJR.07.2970
Lee MW, Lim HK, Kim YJ, Choi D, Kim YS, Lee WJ, et al. Percutaneous sonographically guided radio frequency ablation of hepatocellular carcinoma: causes of mistargeting and factors affecting the feasibility of a second ablation session. J Ultrasound Med 2011;30:607-15. doi: 10.7863/jum.2011.30.5.607. DOI: https://doi.org/10.7863/jum.2011.30.5.607
Kim JE, Kim YS, Rhim H, Lim HK, Lee MW, Choi D, et al. Outcomes of patients with hepatocellular carcinoma referred for percutaneous radiofrequency ablation at a tertiary center: analysis focused on the feasibility with the use of ultrasonography guidance. Eur J Radiol 2011;79:e80-4. doi: 10.1016/j.ejrad.2011.03.090. DOI: https://doi.org/10.1016/j.ejrad.2011.03.090
Song KD, Lee MW, Rhim H, Cha DI, Chong Y, Lim HK. Fusion imaging–guided radiofrequency ablation for hepatocellular carcinomas not visible on conventional ultrasound. AJR Am J Roentgenol 2013;201:1141-7. doi: 10.2214/AJR.13.10532. DOI: https://doi.org/10.2214/AJR.13.10532
Huang HC, Gatchalian LB, Hsieh YC, Chen WT, Lin CC, Lin SM. Real-time virtual sonography-assisted radiofrequency ablation in liver tumors with conspicuous or inconspicuous images or peritumoral landmarks under ultrasonography. Abdom Radiol (NY) 2021;46:2814-22. doi: 10.1007/s00261-020-02875-y. DOI: https://doi.org/10.1007/s00261-020-02875-y
Minami Y, Kudo M. Image guidance in ablation for hepatocellular carcinoma: contrast-enhanced ultrasound and fusion imaging. Front Oncol 2021 ;11:593636. doi: 10.3389/fonc.2021.593636. DOI: https://doi.org/10.3389/fonc.2021.593636
Chernyak V, Fowler KJ, Kamaya A, Kielar AZ, Elsayes K, Bashir MR, et al. Liver Imaging Reporting and Data System (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology 2018 ;289:816–30. doi:10.1148/radiol.2018181494. DOI: https://doi.org/10.1148/radiol.2018181494
Dohmen T, Kataoka E, Yamada I, Miura K, Ohshima S, Shibuya T, et al. Efficacy of contrast-enhanced ultrasonography in radiofrequency ablation for hepatocellular carcinoma. Intern Med 2012;51:1-7. doi: 10.2169/internalmedicine.51.6042. DOI: https://doi.org/10.2169/internalmedicine.51.6042
Rajesh S, Mukund A, Arora A, Jain D, Sarin SK. Contrast-enhanced US-guided radiofrequency ablation of hepatocellular carcinoma. J Vasc Interv Radiol 2013;24:1235-40. doi: 10.1016/j.jvir.2013.04.013. DOI: https://doi.org/10.1016/j.jvir.2013.04.013
Minami Y, Kudo M. Ultrasound fusion imaging technologies for guidance in ablation therapy for liver cancer. J Med Ultrason (2001) 2020;47:257-63. doi: 10.1007/s10396-020-01006-w. DOI: https://doi.org/10.1007/s10396-020-01006-w
Minami Y, Kudo M, Chung H, Inoue T, Takahashi S, Hatanaka K, et al. Percutaneous radiofrequency ablation of sonographically unidentifiable liver tumors. Feasibility and usefulness of a novel guiding technique with an integrated system of computed tomography and sonographic images. Oncology 2007;72 Suppl 1: 111-6. doi: 10.1159/000111716. DOI: https://doi.org/10.1159/000111716
Minami Y, Chung H, Kudo M, Kitai S, Takahashi S, Inoue T, et al. Radiofrequency ablation of hepatocellular carcinoma: value of virtual CT sonography with magnetic navigation. AJR Am J Roentgenol 2008;190:W335-41. doi: 10.2214/AJR.07.3092. DOI: https://doi.org/10.2214/AJR.07.3092
Hirooka M, Luchi H, Kumagi T, Shigematsu S, Hiraoka A, Uehara T, et al. Virtual sonographic radiofrequency ablation of hepatocellular carcinoma visualized on CT but not on conventional sonography. AJR Am J Roentgenol 2006;186(5Suppl):S255-60. doi: 10.2214/AJR.04.1252. DOI: https://doi.org/10.2214/AJR.04.1252
Nakai M, Sato M, Sahara S, Takasaka I, Kawai N, Minamiguchi H, et al. Radiofrequency ablation assisted by real-time virtual sonography and CT for hepatocellular carcinoma undetectable by conventional sonography. Cardiovasc Intervent Radiol 2009;32:62-9. doi: 10.1007/s00270-008-9462-x. DOI: https://doi.org/10.1007/s00270-008-9462-x
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The ASEAN Journal of Radiology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Disclosure Forms and Copyright Agreements
All authors listed on the manuscript must complete both the electronic copyright agreement. (in the case of acceptance)